Brain-body communication
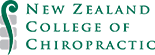
Our next study will focus on how 12-weeks of chiropractic care affects an area of the brain called the prefrontal cortex (PFC). The PFC is a vital area of the brain that impacts:
- metabolic and immunological functions
- mental health
- sleep
- movement
- executive function and
- overall quality of life

This study will be the first of its kind and aims to shed more light on how chiropractic care impacts the health and wellness of so many people around the world. The talented team we’ve assembled to carry out this study spans a number of disciplines and will be utilising innovative advances in technology and machine learning to help us to better understand how chiropractic care impacts nervous system function and human performance.
Watch: Dr Imran Khan Niazi and Dr Heidi Haavik discuss this new study
This study builds on our previous research that showed that a single sessions of chiropractic care affects PFC function. [1] This single session study was a great start, but it didn’t tell us how long this impact on PFC function lasts or how chiropractic care impacts the many vital functions that the PFC controls. The PFC is a vital part of the brain that makes you who you are. It is the part of the brain responsible for your executive function [2-7], it plays a key role in how you experience pain [8-11], is vital for your emotional control and mental health [12-17], and is critically involved in regulating your autonomic nervous system, endocrine system and immune system, enabling you to relax, sleep and heal (see Figure 1) [8, 18-28].
Figure 1: The various vital functions of the prefrontal cortex.
This new study aims to investigate the longer-term effects of chiropractic care on PFC function (12 weeks of care plus 4 weeks follow-up), and to explore which PFC functions may change when someone is adjusted by a chiropractor. To do this, we will assess how chiropractic care affects measures of neurological, metabolic and immunological function, along with mental health, sleep, movement, executive function and health-related quality of life in adults with subclinical pain.
In this parallel-group randomised controlled trial, participants with subclinical pain (120 in total) will be randomly allocated to receive either chiropractic care (n = 60) or a control intervention (n=60). The primary outcomes will include functional near-infrared spectroscopy, heart rate variability and levels of brain-derived neurotrophic factor. This will enable us to assess if chiropractic care causes long-term beneficial changes in PFC function. The secondary outcomes in the study will include other tests of PFC function, such as executive function, measured by multiple cognitive tests, resting-state encephalography, immune and inflammatory markers, sleep and activity levels, mental health, stress and health-related quality of life measures. See Figure 2 for an overview of the project.
The project will be conducted at Railway General Hospital, Pakistan, over the course of a year. The data collected in this project will be a combination of extrinsic (sociodemographic, clinical questionnaires etc.) and intrinsic physiological data (objective physiological measures like EEG, HRV etc.), and will allow us to take advantage of advances in machine learning (also known as artificial intelligence; AI) to help inform the development of optimal chiropractic care plans in the future.
Please help make this project a reality! Please donate today. If everyone gives a little this project can start tomorrow!!!
Figure 2: Overview of study
References
- Lelic, D., et al., Manipulation of dysfunctional spinal joints affects sensorimotor integration in the prefrontal cortex: a brain source localization study. Neural plasticity, 2016. 2016.
- Lelic, D., et al., Manipulation of Dysfunctional Spinal Joints Affects Sensorimotor Integration in the Prefrontal Cortex: A Brain Source Localization Study. Neural Plast, 2016. 2016: p. 3704964.
- Funahashi, S. and J.M. Andreau, Prefrontal cortex and neural mechanisms of executive function. J Physiol Paris, 2013. 107(6): p. 471-82.
- Roberts, A.C., T.W. Robbins, and L.E. Weiskrantz, The prefrontal cortex: executive and cognitive functions. 1998: Oxford University Press.
- Koechlin, E., Prefrontal executive function and adaptive behavior in complex environments. Current Opinion in Neurobiology, 2016. 37: p. 1-6.
- Domenech, P. and E. Koechlin, Executive control and decision-making in the prefrontal cortex. Current opinion in behavioral sciences, 2015. 1: p. 101-106.
- Faw, B., Pre-frontal executive committee for perception, working memory, attention, long-term memory, motor control, and thinking: A tutorial review. Consciousness and cognition, 2003. 12(1): p. 83-139.
- Kul’chyns’kyi, A.B., et al., Causal neuro-immune relationships at patients with chronic pyelonephritis and cholecystitis. correlations between parameters EEG, HRV and white blood cell count. Open Medicine, 2017. 12(1): p. 201-213.
- Lorenz, J., S. Minoshima, and K. Casey, Keeping pain out of mind: the role of the dorsolateral prefrontal cortex in pain modulation. Brain, 2003. 126(5): p. 1079-1091.
- Apkarian, A.V., et al., Human brain mechanisms of pain perception and regulation in health and disease. European Journal of Pain: Ejp, 2005. 9(4): p. 463-84.
- Apkarian, A.V., et al., Chronic Back Pain Is Associated with Decreased Prefrontal and Thalamic Gray Matter Density. The Journal of Neuroscience, 2004. 24(46): p. 10410-10415.
- Arnsten, A.F.T., et al., blair. Neurobiology of Stress, 2015. 1: p. 89-99.
- Eden, A.S., et al., Emotion regulation and trait anxiety are predicted by the microstructure of fibers between amygdala and prefrontal cortex. Journal of Neuroscience, 2015. 35(15): p. 6020-6027.
- Etkin, A., C. Büchel, and J.J. Gross, The neural bases of emotion regulation. Nature reviews neuroscience, 2015. 16(11): p. 693.
- Ghosal, S., B.D. Hare, and R.S. Duman, Prefrontal cortex GABAergic deficits and circuit dysfunction in the pathophysiology and treatment of chronic stress and depression. Current opinion in behavioral sciences, 2017. 14: p. 1-8.
- Johnston-Wilson, N.L., et al., Disease-specific alterations in frontal cortex brain proteins in schizophrenia, bipolar disorder, and major depressive disorder. Molecular Psychiatry, 2000. 5: p. 142.
- Motzkin, J.C., et al., Ventromedial prefrontal cortex is critical for the regulation of amygdala activity in humans. Biological psychiatry, 2015. 77(3): p. 276-284.
- Critchley, Hugo D. and Neil A. Harrison, Visceral Influences on Brain and Behavior. Neuron, 2013. 77(4): p. 624-638.
- Machado, S., et al., Sensorimotor integration: basic concepts, abnormalities related to movement disorders and sensorimotor training-induced cortical reorganization. Rev Neurol, 2010. 51(7): p. 427-436.
- Thayer, J.F., Vagal tone and the inflammatory reflex. Cleve Clin J Med, 2009. 76(Suppl 2): p. S23-6.
- Ahern, G.L., et al., Heart rate and heart rate variability changes in the intracarotid sodium amobarbital test. Epilepsia, 2001. 42(7): p. 912-921.
- Berthoud, H.-R. and W.L. Neuhuber, Functional and chemical anatomy of the afferent vagal system. Autonomic Neuroscience, 2000. 85(1-3): p. 1-17.
- Thayer, J.F. and E.M. Sternberg, Neural aspects of immunomodulation: focus on the vagus nerve. Brain, behavior, and immunity, 2010. 24(8): p. 1223-1228.
- Bankenahally, R. and H. Krovvidi, Autonomic nervous system: anatomy, physiology, and relevance in anaesthesia and critical care medicine. Bja Education, 2016. 16(11): p. 381-387.
- Ohira, H., et al., Vagal nerve activity as a moderator of brain–immune relationships. Journal of Neuroimmunology, 2013. 260(1-2): p. 28-36.
- McCraty, R. and F. Shaffer, Heart rate variability: new perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Global advances in health and medicine, 2015. 4(1): p. 46-61.
- Hänsel, A. and R. Von Känel, The ventro-medial prefrontal cortex: a major link between the autonomic nervous system, regulation of emotion, and stress reactivity? BioPsychoSocial Medicine, 2008. 2(1): p. 21.
- Diorio, D., V. Viau, and M.J. Meaney, The role of the medial prefrontal cortex (cingulate gyrus) in the regulation of hypothalamic-pituitary-adrenal responses to stress. Journal of Neuroscience, 1993. 13(9): p. 3839-3847.